Metformin Hydrochloride Prolonged Release and Glimpiride Tablets - Glucotaj
Glucotaj® M 1mg
Glucotaj® M 2mg
DESCRIPTION
Active Ingredients
Glimepiride and Metformin Hydrochloride (in prolonged release form)
Therapeutic or Pharmacological Class
Antidiabetic
Pharmaceutical Form(s)
Bilayer Tablet (one layer prolonged release)
COMPOSITION
Glucotaj M 1mg
Each uncoated bilayered tablet contains:
Glimepiride IP 1mg
Metformin hydrochloride IP (in prolonged release form) 500mg
Excipients q.s.
Colours : Red Iron Oxide
Glucotaj M 2mg
Each uncoated bilayered tablet contains :
Glimepiride IP 2mg
Metformin hydrochloride IP (in prolonged release form) 500mg
Excipients q.s.
Colours : Yellow Iron Oxide & Indigo Carmine
INDICATION
For the management of patients with type 2 diabetes mellitus when diet, exercise and single agent (glimepiride or metformin alone) do not result in adequate glycemic control.
DOSAGE AND ADMINISTRATION
General
In principle, the dosage of Glucotaj M is governed by the desired blood glucose level. The dosage of Glucotaj M must be the lowest which is sufficient to achieve the desired metabolic control.
During treatment with Glucotaj M glucose levels in blood and urine, must be measured regularly.
In addition, it is recommended that regular determinations of the proportion of glycated haemoglobin be carried out .Mistakes, e.g. forgetting to take a dose, must never be corrected by subsequently taking a larger dose. Measures for dealing with such mistakes (in particular forgetting a dose or skipping a meal) or situations where a dose cannot be taken at the prescribed time must be discussed and agreed between physician and patient beforehand.
For the use only of a Registered Medical Practitioner or Hospital or a Laboratory
This package insert is continually updated. Please read carefully before using a new pack
As an improvement in control of diabetes is, in itself, associated with higher insulin sensitivity,
glimepiride requirements may fall as treatment proceeds. To avoid hypoglycemia timely dose reduction or cessation of Glucotaj M therapy must therefore be considered.
Glucotaj M is to be administered once per day during breakfast or the first main meal.
The highest recommended dose per day should be 8mg of glimepiride and 2000mg of metformin.
Daily doses of glimepiride of more than 6mg are more effective only in a minority of patients. In order to avoid hypoglycemia the starting dose of Glucotaj M should not exceed the daily doses of glimepiride or metformin already being taken.
When switching from combination therapy of glimepiride plus metformin as separate tablets, Glucotaj M should be administered on the basis of dosage currently being taken.
Titration:
The daily dose should be titrated based on the glycemic control ,in increments of 1 tablet only, corresponding to the lowest strength. Duration of therapy: Treatment with Glucotaj M is normally a long-term therapy.
Special Populations :
Children
Data are insufficient to recommend pediatric use of Glucotaj M.
Renal impairment
A GFR should be assessed before initiation of treatment with metformin containing products and at least annually thereafter. In patients at increased risk of further progression of renal impairment and in the elderly, renal function should be assessed more frequently, e.g. every 3-6 months.The maximum daily dose of metformin should preferably be divided into 2-3 daily doses.
Factors that may increase the risk of lactic acidosis (see Section Warnings) should be reviewed before considering initiation of metformin in patients with GFR<60 mL/min.
If no adequate strength of Glucotaj M is available, individual monocomponents should be used instead of the fixed dose combination. GFR ml/min Metformin Glimepride 60-89 Maximum daily dose is 3000 mg Dose reduction may be considered in relation to declining renal function. The highest recommended dose per day should be 8 mg of glimepiride 45-59 Maximum daily dose is 2000 mg The starting dose is at most half of the maximum dose. 30-44 Maximum daily dose is 1000 mg.
The starting dose is at most half of the maximum dose.
30 Metformin is contraindicated Change-over to insulin is indicated, not least to achieve optimal metabolic control
ADMINISTRATION
Due to prolonged release formulation, Glucotaj M must be swallowed whole and not crushed or chewed.
CONTRAINDICATIONS:
For Glimepiride:
in patients hypersensitive to glimepiride, other sulfonylureas, other sulfonamides, or any of the excipients of Glucotaj® M in pregnant women. in breast-feeding women.
patients with severe impairment of liver function and in dialysis patients. In patients with severe impairment of hepatic function, change-over to insulin is indicated, not least to achieve optimal metabolic control.
For Metformin:
Hypersensitivity to metformin or any of the excipients. Any type of acute metabolic acidosis (such as lactic acidosis,diabetic ketoacidosis, diabetic pre-coma).
Severe renal failure (GFR 30ml/min)
Acute conditions with the potential to alter renal function such as:
- Dehydration
- severe infection
- shock
- Intravascular administration of iodinated contrast agents (see Precautions)
Acute or chronic disease which may cause tissue hypoxia such as: -cardiac or respiratory failure
- recent myocardial infarction
- shock
Hepatic insufficiency
Acute alcohol intoxication, alcoholism.
Lactation.
WARNINGS
For Glimepiride:
In exceptional stress situations (e.g. trauma, surgery, febrile infections) blood glucose regulation may deteriorate, and a temporary change to insulin may be necessary to maintain good metabolic control.
For Metformin:
Lactic acidosis
Metformin accumulation occurs at acute worsening of renal function and increases the risk of lactic acidosis.
In case of dehydration (severe diarrhoea or vomiting, fever or reduced fluid intake), metformin should be temporarily discontinued and contact with a health care professional is recommended.
Medicinal products that can acutely impair renal function (such as antihypertensives, diuretics and NSAIDs) should be initiated with caution in metformin-treated patients. Other risk factors associated to lactic acidosis are excessive alcohol intake,hepatic insufficiency, inadequately controlled diabetes, ketosis, prolonged fasting,and any conditions associated with hypoxia as well as concomitant use of medicinal products that may cause lactic acidosis (see Section Contraindications and Section Interactions) Diagnosis: Patients and/or care-givers should be informed of the risk of lactic acidosis. In case of suspected symptoms, the patient should stop taking metformin and seek immediate medical attention. Diagnostic laboratory findings are decreased blood pH,( 7.35), increased plasma lactate levels ( 5 mmol/L), and an increased anion gap and lactate/pyruvate ratio.
Renal function:
GFR should be assessed before treatment initiation and regularly thereafter (see Section Dosage and Administration).
Metformin is contraindicated in patients with GFR<30 ml/min and should be temporarily discontinued in the presence of conditions that alter renal function, (see Section Contraindications) Decreased renal function in elderly subjects is frequent and asymptomatic. Special caution should be exercised in situations where renal function may become impaired, for example when initiating antihypertensive therapy or diuretic therapy and when starting therapy with an NSAID.
Administration of iodinated contrast agent:
Intravascular administration of iodinated contrast agents may lead to contrast induced nephropathy, resulting in metformin accumulation and an increased risk of lactic acidosis.
Metformin should be discontinued prior to, or at the time of the imaging procedure and not restarted until 48 hours after, provided that renal function has been re-evaluated and found to be stable (see Section Dosage and Administration and Section Interactions).
Surgery:
Metformin must be discontinued at the time of surgery under general ,spinal or epidural anaesthesia.Therapy may be restarted no earlier than 48 hours following surgery or resumption of oral nutrition and provided that renal function has been re-evaluated and found to be stable.
PRECAUTIONS
For Glimepiride:
In the initial weeks of treatment, the risk of hypoglycaemia may be increased and necessitates especially careful monitoring. Factors favouring hypoglycaemia include:
unwillingness or (more commonly in older patients) incapacity of the patient to cooperate.
undernourishment, irregular mealtimes or skipped meals. imbalance between physical exertion and carbohydrate intake. alterations of diet.
consumption of alcohol, especially in combination with skipped meals.
impaired renal function.
severe impairmentof liver function.
overdose with glimepiride.
certain uncompensated disorder of the endocrine system affecting carbohydrate metabolism or counter - regulation of hypoglycaemia ( as for example in certain disorders of thyroid functionand in anterior pituitary or corticoadrenal insufficiency. )
concurrent administration of certain other medicines (see Interactions). treatment with glimepiride in the absence of any indication.
If such risk factors for hypoglycaemia are present, it may be necessary to adjust the dosage of glimepiride or the entire therapy. This also applies whenever illness occurs during therapy or the patient's life-style changes. Those symptoms of hypoglycaemia which reflect the body's adrenergic counter regulation (see Adverse Reactions) may be milder or absent where hypoglycaemia develops gradually, in the elderly, and where there is autonomic neuropathy or where the patient is receiving concurrent treatment with beta-blockers, clonidine, reserpine, guanethidine or other sympatholytic drugs. Hypoglycaemia can almost always be promptly controlled by immediate intake of carbohydrates(glucose or sugar). It is known from other sulfonylureas that, despite initially successful countermeasures, hypoglycaemia may recur. Patients must, therefore, remain under close observation. Severe hypoglycaemia further requires immediate treatment and follow-up by a physician and, in some circumstances, in-patient hospital care.
Treatment of patients with G6PD-deficiency with sulfonylurea agents can lead to hemolytic anaemia. Since glimepiride belongs to the class of sulfonylurea agents, caution should be used in patients with G6PDdeficiency and a non-sulfonylurea alternative should be considered.
For Metformin:
Regular monitoring of thyroid-stimulating hormone (TSH) levels is recommended in patients with hypothyroidism (see Adverse reactions) Long-term treatment with metformin has been associated with a decrease in vitamin B12 serum levels which may cause peripheral neuropathy. Monitoring of the vitamin B12 level is recommended (see Adverse reactions)
Other precautions:
All patients should continue their diet with a regular distribution of carbohydrate intake during the day. Overweight patients should continue their energy-restricted diet.
The usual laboratory tests for diabetes monitoring should be performed regularly.
Metformin alone never causes hypoglycaemia, although caution is advised when it is used in combination with insulin or sulfonylureas.
INTERACTIONS
For Glimepiride:
Based on experience with glimepiride and on what is known of other sulfonylureas, the following interactions must be considered: Glimepiride is metabolized by cytochrome P450 2C9 (CYP2C9). This should be taken into account when glimepiride is coadministered with inducers (e.g. rifampicin) or inhibitors (e.g. fluconazole) of CYP2C9. Potentiation of the blood-glucose-lowering effect and, thus, in some instances hypoglycaemia may occur when one of the following drugs is taken, for example: insulin and other oral antidiabetics; ACE inhibitors; anabolic steroids and male sex hormones; chloramphenicol;
fenyramidol; fibrates; fluoxetine; guanethidine; ifosfamide; MAO inhibitors; miconazole; fluconazole; paraaminosalicylic acid; pentoxifylline (high dose parenteral); phenylbutazone; azapropazone; oxyphenbutazone; probenecid; quinolones; salicylates; sulfinpyrazone; clarithromycin; sulfonamide antibiotics; tetracyclines; tritoqualine; trofosfamide. Weakening of the blood-glucose-lowering effect and, thus raised blood glucose levels may occur when one of the following drugs is taken, for example: acetazolamide; barbiturates; corticosteroids; diazoxide; diuretics; epinephrine (adrenaline) and other sympathomimetic agents; glucagon; laxatives (after protracted use); nicotinic acid (in high doses); oestrogens and progestogens; phenothiazines; phenytoin; rifampicin; thyroid hormones.
H2 receptor antagonists, beta-blockers, clonidine and reserpine may lead to either potentiation or weakening of the blood glucose-lowering effect. Under the influence of sympatholytic drugs such as beta-blockers, clonidine, guanethidine and reserpine, the signs of adrenergic counterregulation to hypoglycaemia may be reduced or absent.
Both acute and chronic alcohol intake may potentiate or weaken the blood glucose-lowering action of glimepiride in an unpredictable fashion. The effect of coumarin derivatives may be potentiated or weakened.
Bile acid sequestrant: Colesevelam binds to glimepiride and reduces glimepiride absorption from the gastro-intestinal tract. No interaction was observed when glimepiride was taken at least 4 hours before colesevelam. Therefore glimepiride should be administered at least 4 hours prior to colesevelam
For Metformin:
Concomitant use not recommended:
Alcohol: Alcohol intoxication is associated with an increased risk of lactic acidosis, particularly in case of fasting or malnutrition or hepatic insufficiency.
Avoid consumption of alcohol and alcohol-containing medications. Iodinated contrast agents Metformin must be discontinued prior to, or at the time of the image procedure and not restarted until at least 48 hours after, provided that renal function has been reevaluated and found to be stable(See Section Dosage and Administration and Warnings).
Combinations requiring precautions for use:
Some medicinal products can adversely affect renal function which may increase the risk of lactic acidosis, e.g. NSAIDs, including selective cyclo-oxygenase (COX) II inhibitors, ACE inhibitors, angiotensin II receptor antagonists and diuretics, especially loop diuretics. When starting or using such products in combination with metformin, close monitoring of renal function is necessary.
Glucocorticoids (systemic and local routes), beta-2-agonists and diuretics have intrinsic hyperglycaemic activity. Inform the patient and perform more frequent blood glucose monitoring, especially at the beginning of treatment. If necessary, adjust the dosage of the antidiabetic drug during therapy with the other drug and upon its discontinuation. ACE-inhibitors may decrease the blood glucose levels. If necessary, adjust the dosage of the antidiabetic drug during therapy with the other drug and upon its discontinuation.
Metformin may decrease the anticoagulant effect of phenprocoumon. Therefore, a close monitoring of the INR is recommended. Levothyroxine can reduce the hypoglycemic effect of metformin. Monitoring of blood glucose levels is recommended, especially when thyroid hormone therapy is initiated or stopped, and the dosage of metformin must be adjusted if necessary.
Organic cation transporters (OCT)
Metformin is a substrate of both transporters OCT1 and OCT2. Co-administration of metformin with
• Inhibitors of OCT1 (such as verapamil) may reduce efficacy of metformin.
• Inducers of OCT1 (such as rifampicin) may increase gastrointestinal absorption and efficacy of metformin.
• Inhibitors of OCT2 (such as cimetidine, dolutegravir, ranolazine, trimethoprime, vandetanib, isavuconazole) may decrease the renal elimination of metformin and thus lead to an increase in metformin plasma concentration.
• Inhibitors of both OCT1 and OCT2 (such as crizotinib, olaparib) may alter efficacy and renal elimination of metformin. Caution is therefore advised, especially in patients with renal impairment, when these drugs are coadministered with metformin, as metformin plasma concentration may increase. If needed, dose adjustment of metformin may be considered as OCT inhibitors/inducers may alter the efficacy of metformin
PREGNANCY
For Glimepiride:
Glimepiride must not be taken during pregnancy. Otherwise there is risk of harm to the child. The patient must change over to insulin during pregnancy.
Patients planning a pregnancy must inform their physician. It is recommended that such patients change over to insulin.
For Metformin:
To date, no relevant epidemiological data are available. Animal studies do not indicate harmful effects with respect to pregnancy, embryonal or fetal development, parturition or postnatal development.
When the patient plans to become pregnant and during pregnancy, diabetes should not be treated with metformin but insulin should be used to maintain blood glucose levels as close to normal as possible in order to lower the risk of fetal malformations associated with abnormal blood glucose levels.
LACTATION
For Glimepiride:
To prevent possible ingestion with the breast milk and possible harm to the child, glimepiride must not be taken by breast-feeding women. If necessary the patient must change over to insulin, or must stop breastfeeding.
For Metformin:
Metformin is excreted into milk in lactating rats. Similar data is not available in humans and a decision should be made whether to discontinue nursing or to discontinue metformin, taking into account the importance of the compound to the mother.
DRIVING A VEHICLE OR PERFORMING OTHER HAZARDOUS TASKS
For Glimepiride:
Alertness and reactions may be impaired due to hypo- or hyperglycemia, especially when beginning or after altering treatment or when glimepiride is not taken regularly. This may, for example, affect the ability to drive or to operate machinery.
For Metformin:
Metformin monotherapy does not cause hypoglycaemia and therefore has no effect on the ability to drive or to use machines. However, patients should be alerted to the risk of hypoglycaemia when metformin is used in combination with other antidiabetic agents (sulfonylureas, insulin, repaglinide).
ADVERSE REACTIONS
The following CIOMS frequency rating is used, when applicable : Very common ≥10%; Common ≥1 and <10%; Uncommon ≥0.1 and <1%; Rare ≥0.01 and <0.1%; Very rare<0.01%, Unknown ( cannot be estimated from available data). For Glimepiride and Metformin The use of a combination of both compounds, either as a free combination or as a fixed combination, is associated with the same safety characteristics as the use of each compound separately.
For Glimepiride:
Metabolism and nutrition disorders
As a result of the blood-glucose-lowering action of glimepiride, hypoglycaemia may occur, which may also be prolonged.
Possible symptoms of hypoglycaemia include headache, ravenous hunger, nausea, vomiting, lassitude, sleepiness, disordered sleep, restlessness, aggressiveness, impaired concentration, impaired alertness and reactions, depression, confusion, speech disorders, aphasia, visual disorders, tremor, pareses, sensory disturbances, dizziness, helplessness, loss of self-control, delirium, cerebral convulsions, somnolence and loss of consciousness up to and including coma, shallow respiration and bradycardia.
In addition, signs of adrenergic counter-regulation may be present such as sweating, clammy skin, anxiety, tachycardia, hypertension, palpitations, angina pectoris, and cardiac arrhythmias.
The clinical picture of a severe hypoglycaemic attack may resemble that of a stroke.
The symptoms nearly always subside when hypoglycaemia is corrected. Eye disorders Especially at the start of treatment, there may be temporary visual impairment due to the change in blood glucose levels. The cause is a temporary alteration in the turgidity and hence the refractive index of the lens, this being dependent on blood glucose level.
Gastrointestinal disorders
sensations of pressure or fulness in the epigastrium, abdominal pain and diarrhoea may occur. In isolated cases, there may be hepatitis, elevation of liver enzyme levels and/or cholestasis and jaundice, which may progress to life-threatening liver failure but can regress after withdrawal of glimepiride.
Dysgeusia (frequency not known)
Blood and lymphatic system disorders
Changes in the blood picture may occur: Rarely, thrombocytopenia and, in isolated cases, leucopenia, haemolytic anaemia, erythrocytopenia, granulocytopenia, agranulocytosis or pancytopenia may develop. Cases of severe thrombocytopenia with platelet count less than 10,000/ l and thrombocytopenic purpura have been reported in post-marketing experience (frequency not known).
Skin and subcutaneous tissue disorders
Alopecia (frequency not known)
General disorders
Occasionally, allergic or pseudoallergic reactions may occur, e.g. in the form of itching, urticaria or rashes. Such mild reactions may develop into serious reactions with dyspnoea and a fall in blood pressure, sometimes progressing to shock. In the event of urticaria a physician must therefore be notified immediately.
In isolated cases, a decrease in serum sodium concentration and allergic vasculitis or hypersensitivity of the skin to light may occur.
Investigations
Glimepiride,like all sulfonylureas , can cause weight gain (frequency not known)
For Metformin:
Gastrointestinal symptoms such as nausea, vomiting, diarrhoea, abdominal pain and loss of appetite (>10%) are very common: these occur most frequently during initiation of therapy and resolve spontaneously in most cases. To prevent these gastrointestinal symptoms, it is recommended that metformin be taken in 2 or 3 daily doses during or after meals. A slow increase of the dose may also improve gastrointestinal tolerability.
- Metallic taste (3%) is common.
- Mild erythema has been reported in some hypersensitive individuals. The incidence of such effects is regarded as very rare (<0.01%).
been observed in patients treated long-term with metformin and appears generally to be without clinical significance (<0.01%).
However, cases of peripheral neuropathy in patients with vitamin B12 deficiency have been reported in post-marketing experience (frequency not known) (see Precautions)
-Lactic acidosis (0.03 cases/1000 patient-years) is very rare (see Warnings).
- Hemolytic anemia (frequency unknown)
- Reduction of thyrotropin level in patients with hypothyroidism (see Precautions) (frequency unknown)
- Hypomagnesemia in the context of diarrhea (frequency unknown)
- Encephalopathy (frequency unknown)
- Photosensitivity (frequency unknown)
- Hepatobiliary disorders: Reports of liver function tests abnormalities and hepatitis resolving upon metformin discontinuation
OVERDOSAGE:
For Glimepiride:
Signs and Symptoms:
Acute overdosage as well as long-term treatment with too high a dose of glimepiride may lead to severe life-threatening hypoglycaemia.
Management:
As soon as an overdose of glimepiride has been discovered, a physician must be notified without delay. The patient must immediately take sugar, if possible in the form of glucose, unless a physician has already undertaken responsibility for treating the overdose. Careful monitoring is essential until the physician is confident that the patient is out of danger. It must be remembered that hypoglycaemia may recur after initial recovery. Admission to hospital may sometimes be necessary - even as a precautionary measure.
In particular, significant overdoses and severe reactions with signs such as loss of consciousness or other serious neurological disorders are medical emergencies and require immediate treatment and admission to hospital.
If, for example, the patient is unconscious, an intravenous injection of concentrated glucose solution is indicated (for adults starting with 40 ml of 20% solution, for example). Alternatively in adults, administration of glucagon, e.g. in doses of 0.5 to 1 mg i.v., s.c. or i.m. may be considered.
In particular when treating hypoglycaemia due to accidental intake of glimepiride in infants and young children, the dose of glucose given must be very carefully adjusted in view of the possibility of producing dangerous hyperglycaemia, and must be controlled by close monitoring of blood glucose.
Patients who have ingested life-threatening amounts of glimepiride require detoxification (e.g. by gastric lavage and medicinal charcoal). After acute glucose replacement has been completed it is usually necessary to give an intravenous glucose infusion in lower concentration so as to ensure that the hypoglycaemia does not recur. The patient's blood glucose level should be carefully monitored for at least 24 hours. In severe cases with a protracted course, hypoglycaemia, or the danger of slipping back into hypoglycaemia, may persist for several days.
For Metformin:
Hypoglycaemia has not been seen with metformin doses of up to 85 g, although lactic acidosis has occurred in such circumstances. High overdose or concomitant risks of metformin may lead to lactic acidosis. Lactic acidosis is a medical emergency and must be treated in hospital. The most effective method to remove lactate and metformin is haemodialysis. Pancreatitis may occur in the context of a metformin overdose
STORAGE CONDITIONS
Store below +25°C in a dry place.
Keep out of reach of children.
Manufactured in India by:
TAJ PHARMACEUTICALS LTD.
Mumbai, India
Unit no 214.Old Bake House
Maharashtra Chambers of Commerce Lane,
Fort, Mumbai - 400001
at : Ahmedabad-382213, Gujarat, INDIA.
Code No.: GUJ/DRUGS/G/25A/4795-A
Updated : May 2019
Reference: CCDS Version 11 dated 17th October 2017 for Glimepiride plus
Metformin Fixed Dose Combination
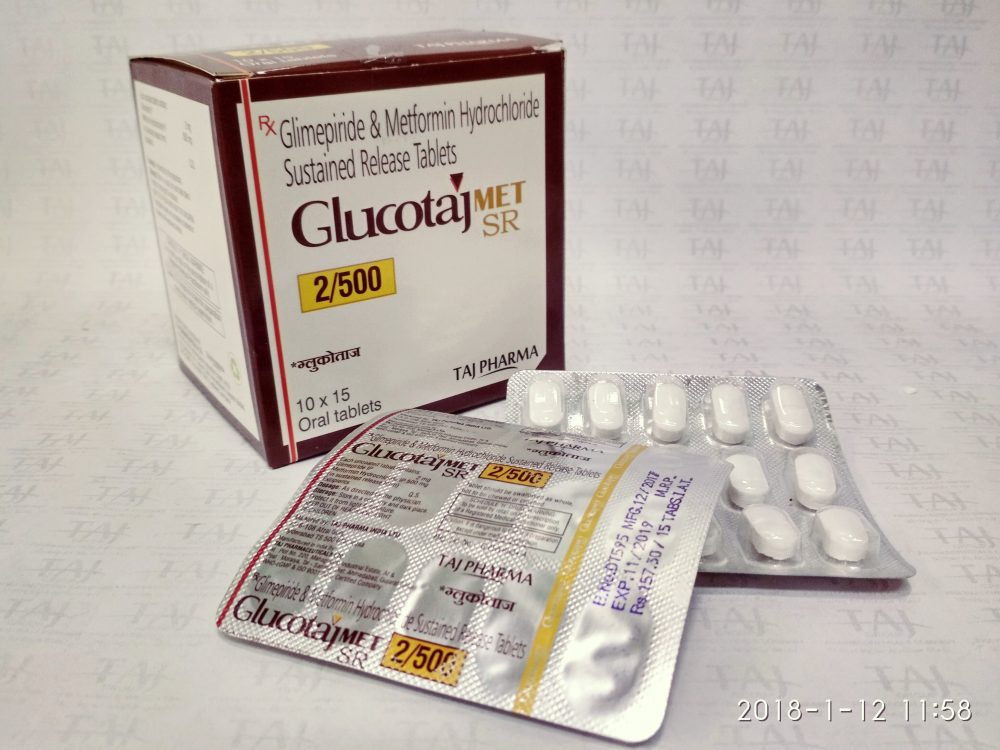
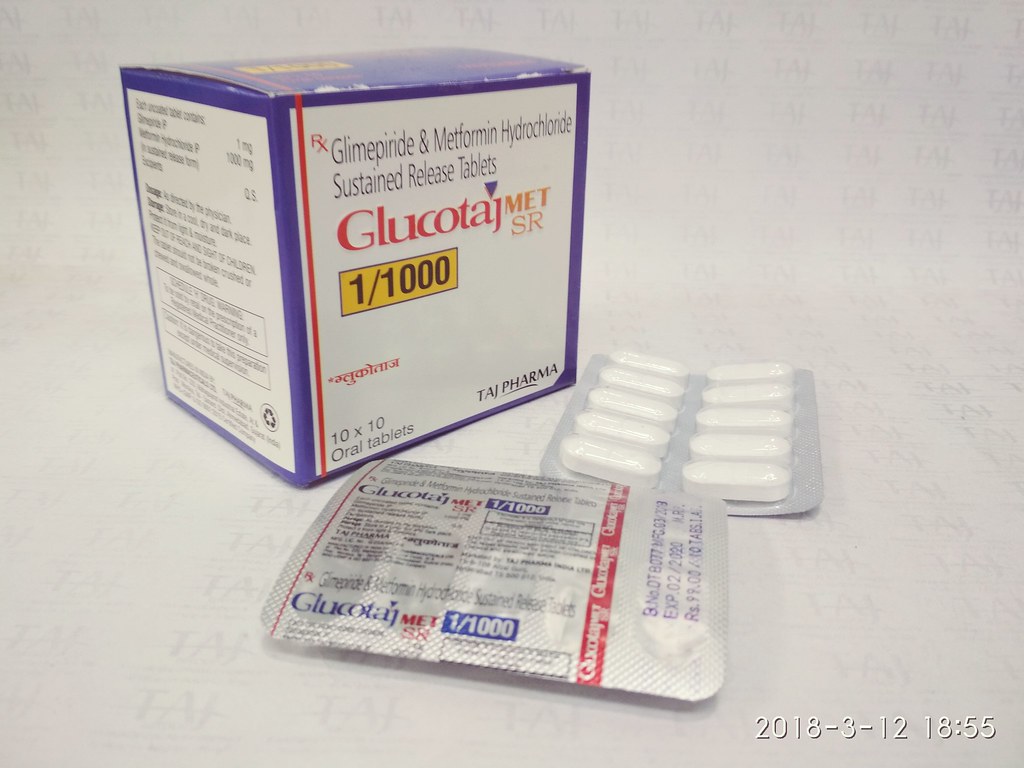
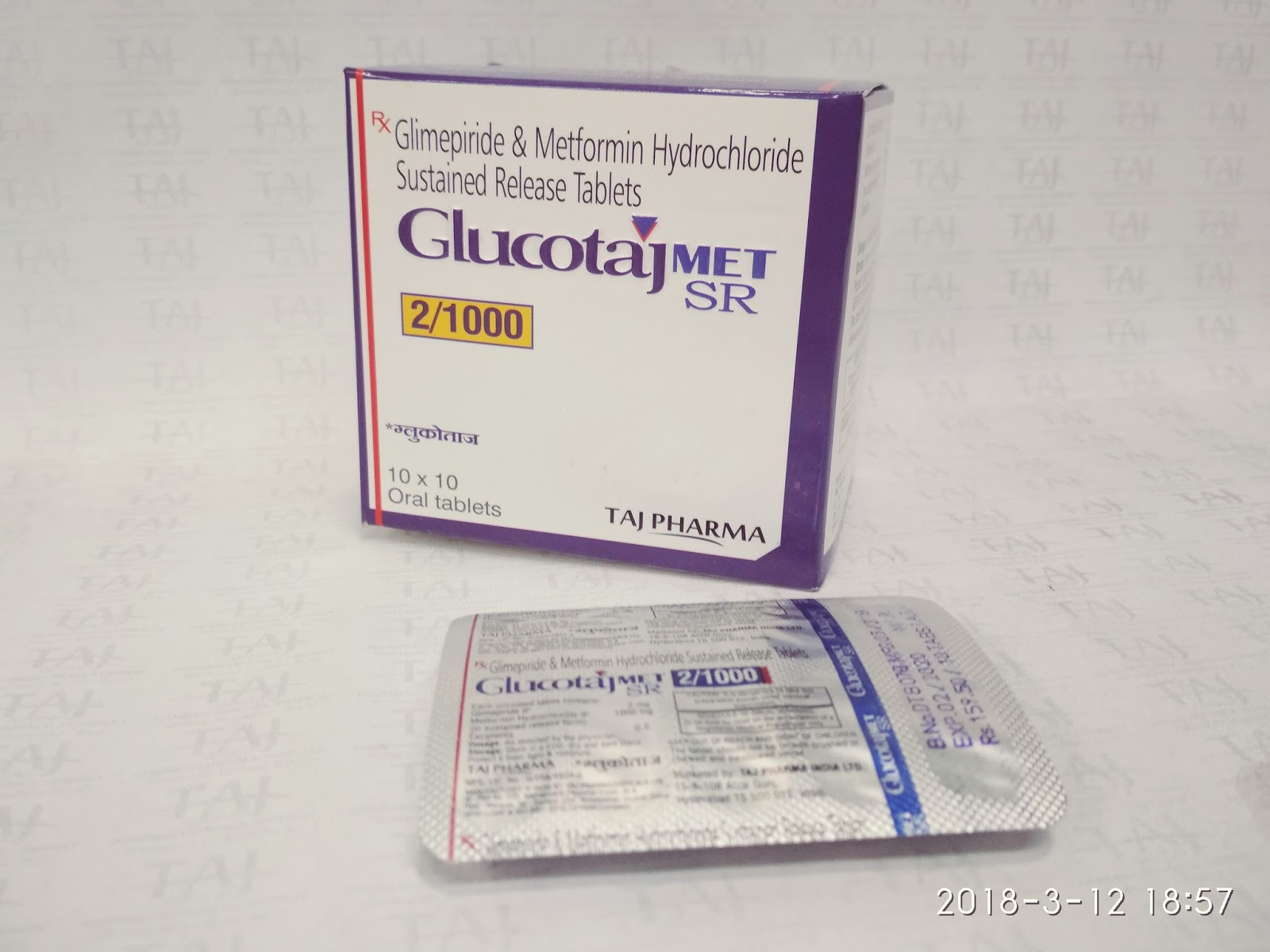
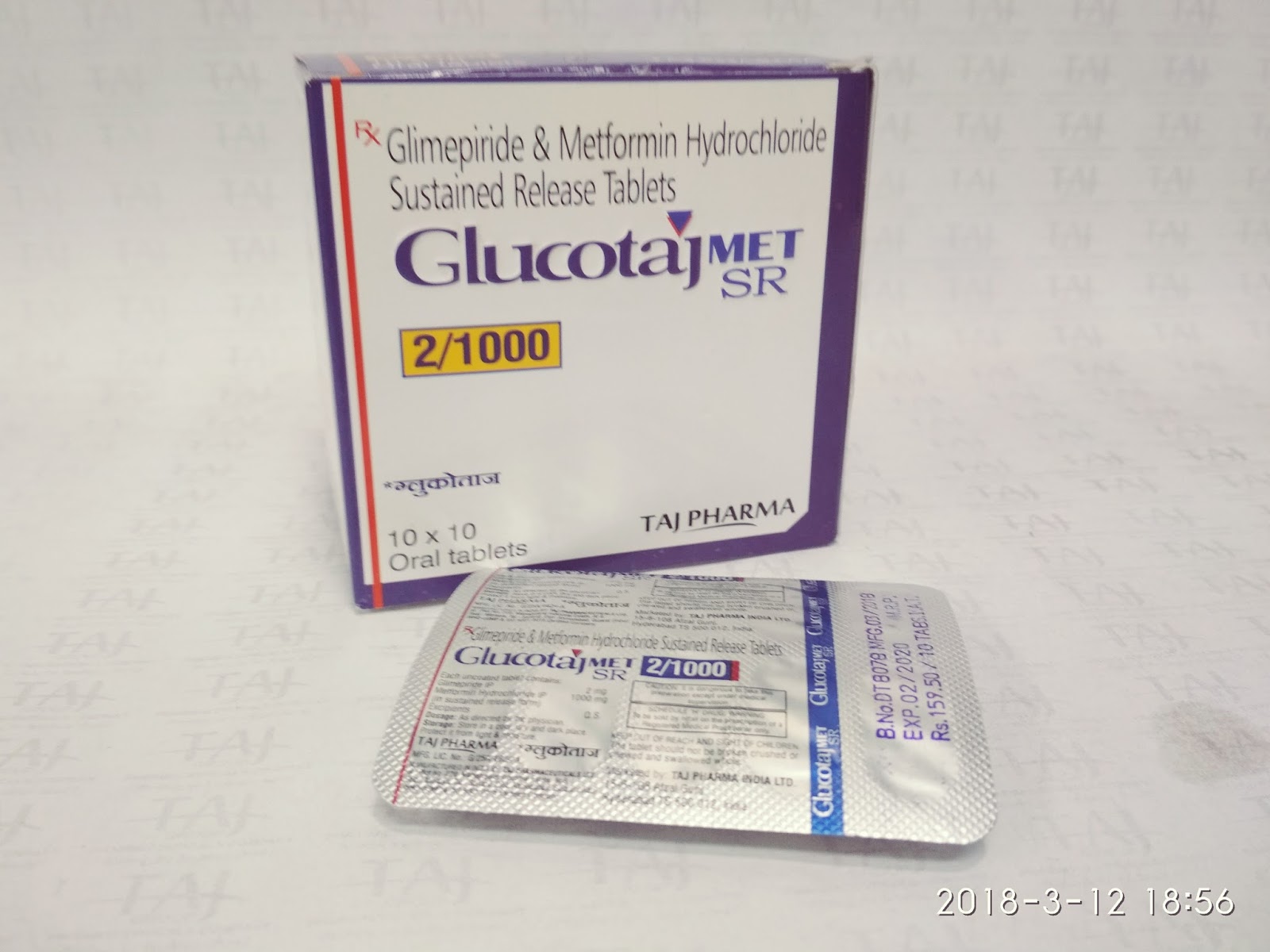
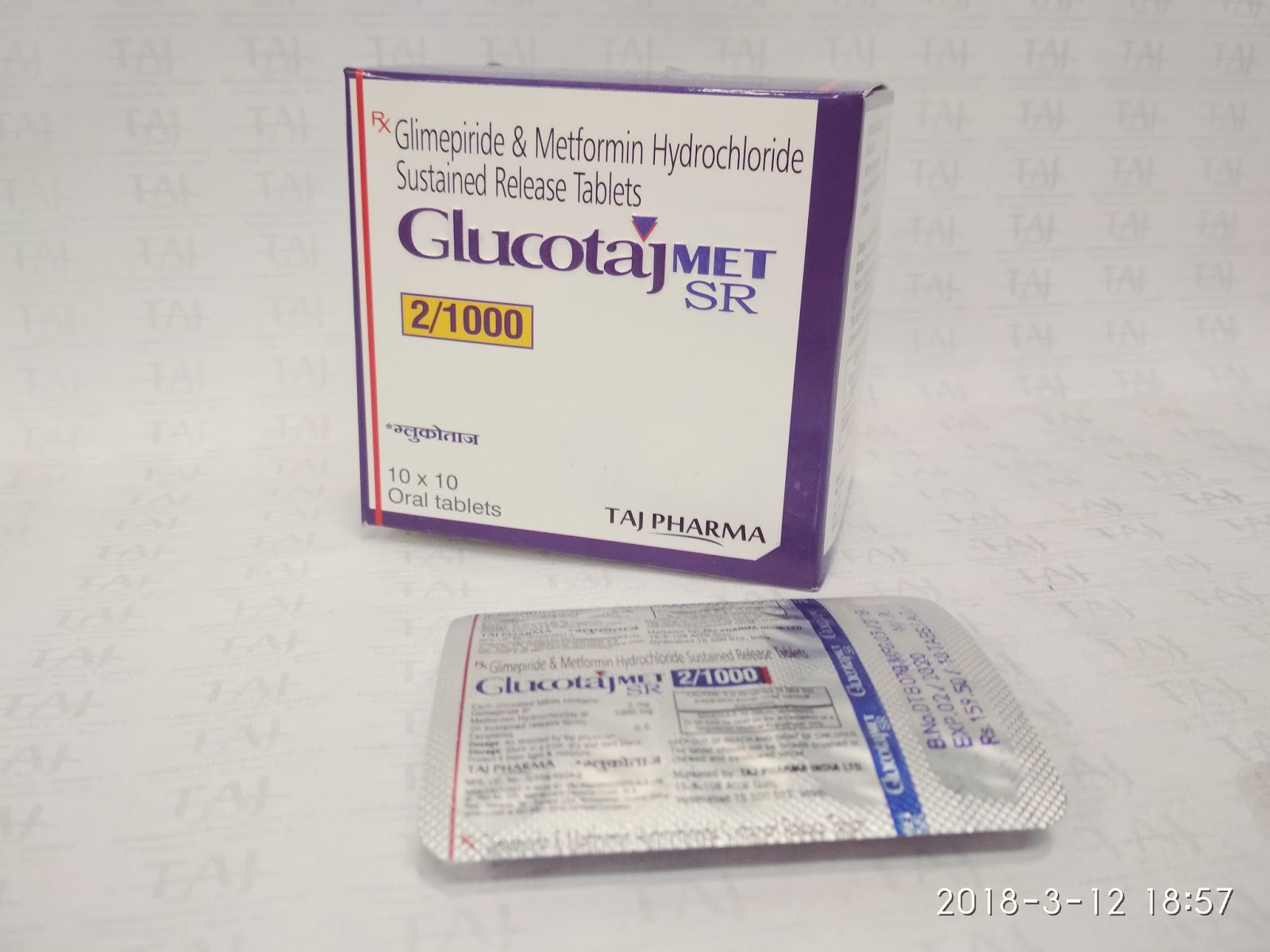
Glucotaj Image Gallery
Here you can see the images of Metformin Hydrochloride Prolonged Release and Glimpiride Tablets.
Our Partners
A dream for new world Anchored in India and committed to its traditional values of leadership with trust, the Taj Pharma Group is spreading its footprint globally through excellence and innovation. Taj Pahrma







Life is the underlying purpose of everything we do at Taj Pharma Group. We are committed to developing a distinguished generics pharmaceuticals business.
Taj Pharma is one of the leading generic pharmaceutical company in India. We hold top positions in different established markets and gradually building a strong presence in many emerging generics markets. We have eight manufacturing sites under flagship in India to support our market standing.
Copyright © Taj Pharmaceuticals Limited. All rights reserved. by Taj Pharma Group India.
Note: This site contains medical information that is intended for doctors or medical practitioner only and is not meant to substitute for the advice provided by a medical professional. Always consult a physician if you have health concerns. Use and access of this site is subject to the terms and conditions as set out in our Privacy Policy and Terms of Use. Copyright © Taj Pharmaceuticals Limited (India), All Rights Reserved.