Metformin Hydrochloride Prolonged Release and Glimpiride Tablets - Glucotaj
1 Name of the medicinal product
Glimepiride + Metformin
2 Qualitative and quantitative composition
One tablet contains:
Active substances: Glimepiride micronized - 2 mg, Metformin hydrochloride - 500 mg; Excipients: Lactose monohydrate - 50 mg, Carboxymethyl starch sodium - 15 mg, Povidone K30 - 25 mg Microcrystalline cellulose - 50 mg, Crospovidone - 10 mg, Magnesium stearate - 5 mg; Film coating: Hypromellose - 9.4 mg, Macrogol-6000 - 1.7 mg, Titanium dioxide (E 171) - 1.7 mg, Carnauba wax - 0.2 mg.
3 Pharmaceutical form
Tablets 2 mg + 500 mg
Oval biconvex tablets, film-coated, white
4 Clinical particulars
4.1 Therapeutic indications
Treatment of diabetes mellitus type 2 (in addition to diet, physical exercise and weight loss):
- When glycemic control cannot be achieved with metformin or glimepiride monotherapy;
- In case of replacement of combination therapy of glimepiride and metformin monotherapy in order to administer a combined medicine Amaril®M.
4.2 Posology and method of administration
Typically the dose of medicine Glucotaj should be determined by the target glucose concentration in blood. It is necessary to take the lowest dose that would be sufficient to achieve the desired metabolic control.
During treatment with medicine Glucotaj, concentration of glucose in blood should be regularly determined. In addition, regular control of percentage of glycated hemoglobin is also recommended.
Incorrect administration of the medicine, such as skipping of the next dose, should never be replenished by subsequent administration of higher doses.
Actions of the patient in case of mistakes while taking the medicine (in particular in case of skipping of the next dose of Glucotaj or skipping of a meal), or in the situations where there is no possibility to take the medicine, should be consulted in advance between the patient and the physician.
Since improvement in metabolic control is associated with increased sensitivity of tissues to insulin, the need for glimepiride may decrease in the course of treatment with Glucotaj. In order to avoid development of hypoglycemia, the dose should be promptly reduced or administration of Glucotaj should be stopped.
Glucotaj should be taken once or twice a day during a meal.
Maximum single dose of metformin is 1000 mg.
Maximum daily dose: 8 mg - for glimepiride and 2 000 mg – for metformin.
Only for a small number of patients more effective daily dose is more than 6 mg of glimepiride.
Initial dose of Glucotaj should not exceed daily dose of glimepiride and metformin already being taken by a patient in order to avoid hypoglycemia. When transferring patients taking the combination of glimepiride and metforminmonotherapies to Glucotaj, dose of Glucotaj will be determined on the basis of doses of glimepiride and metformin taken already, as separate preparations.
If increase of the dose is necessary, daily dose of Glucotaj should be titrated in increments of only 1 tablet of Glucotaj 1 mg + 250 mg or ½ tablet of Glucotaj 2 mg + 500 mg.
Duration of treatment
Typically, treatment with Glucotaj is carried out for a long time.
Use in pediatric patients
Safety and efficacy of the medicine was not studied in children with diabetes mellitus type 2.
Use in elderly patients
Metformin is excreted mainly by the kidneys. Since there is the risk of development of severe adverse reactions to metformin in patients with impaired renal function, the medicine can only be used in patients with normal renal function. Due to the fact that renal function is reduced with age, metformin should be used with caution. You should carefully select the dose and ensure thorough and regular monitoring of renal function.
4.3 Contraindications
- Diabetes mellitus type 1;
- Diabetic ketoacidosis including history of diabetic coma and precoma, acute or chronic metabolic acidosis;
- Increased sensitivity to sulfonylureas, sulfonamides or biguanides, as well as any of the excipients of the medicine;
- Severe hepatic dysfunction (lack of experience of administration; in order to provide adequate glycemic control, such patients should be treated with insulin);
- Patients on hemodialysis (lack of experience of administration);
- Renal insufficiency and renal failure (creatinine concentration in blood plasma: ≥ 1.5 mg/dL (135 mkmol/l) in men and ≥ 1.2 mg/dL (110 mkmol/l) in women or reduction in creatinine clearance (increased risk of development of lactic acidosis and other side effects of metformin);
- Acute condition, during which impairment of renal function may be suspected (dehydration, severe infection, shock, intravascular administration of iodinated contrast agents (see “Special indications”);
- Acute and chronic disease which may cause tissue hypoxia (cardiac or respiratory failure, acute and subacute myocardial infarction, shock);
- Tendency to development of lactic acidosis, lactic acidosis in history;
- Stressful situations (severe trauma, burns, surgery, severe infection with fever, septicemia);
- Exhaustion, starvation, being on hypocaloric diet (less than 1000 calories/day);
- Violation of absorption of food and drugs in the gastrointestinal tract (in case of bowel obstruction, intestinal paresis, diarrhea, vomiting);
- Chronic alcoholism, acute poisoning with alcohol.
- Lactase deficiency, lactose intolerance, glucose-galactosemalabsorption;
- Pregnancy, planning to become pregnant;
- Period of breast-feeding.
- Children and adolescents under 18 years of age (lack of clinical experience).
4.4 Special Warnings and precautions for use
- Particularly careful monitoring of the glucose concentration in the blood is required in the first weeks of treatment with Glucotaj, because of the risk of hypoglycemia, especially in the following conditions, under which risk of hypoglycaemia is increased:
- Unwillingness or inability of the patient to cooperate with the physician [most often this is shown in the elderly patients);
- Lack of nutrition, regular food intake, omission of meals;
- Incompliance between physical activity and carbohydrate intake;
- Changes in diet;
- Use of alcoholic beverage, especially in combination with omission of meals;
- Liver and kidney insufficiency;
- Certain uncompensated endocrine disorders such as thyroid disorders, lack of hormones of the anterior pituitary or the adrenal cortex, affecting carbohydrate metabolism or activation of mechanisms aimed at increase of glucose concentration in the blood during hypoglycemia;
- Treatment with glimepiride in the absence of any indication;
- Over-dosage of glimepiride;
- Development of intercurrent disease during treatment or lifestyle changes;
In these cases, more careful control of blood glucose concentrations and hypoglycemia symptoms is required, dose adjustment of Glucotaj or the entire hypoglycemic therapy may become necessary.
- In case of concomitant treatment with other medicinal products (see “Interaction with other medicinal products”);
- With simultaneous use of certain medicinal products (see “Interaction with other medicinal products”);
- Elderly patients (in these cases asymptomatic decrease in kidney function is often observed);
- In the situations where renal function may deteriorate, such as starting of administration of antihypertensive medicines or diuretics, as well as non-steroid anti-inflammatory drugs (NSAIDs) by a patient (increased risk of lactic acidosis and other side effects of metformin);
- When performing heavy physical exercise (risk of development of lactic acidosis while taking metformin is increased);
- In case of lack of symptoms of adrenergic anti-hypoglycemic regulation in response to developing hypoglycemia (in elderly patients, with autonomic neuropathy or simultaneous therapy with beta-blockers, clonidine, guanethidine, reserpine and other sympatholitics) (more careful monitoring of blood glucose concentrations is required in these patients); - In case of in sufficiency of glucose-6-phosphate dehydrogenase (when receiving sulfonylureas, hemolytic anemia may develop in these patients, therefore administration of alternative hypoglycemic drugs, non-sulfonylurea, should be considered).
4.5 Interaction with other medicinal products and other forms of interaction
Interaction of glimepiride with other pharmaceutical products
Adverse reactions may develop in case of simultaneous administration of glimepiride with other pharmaceutical products: enhancement or reduction of its hypoglycemic action. Based on clinical experience with glimepiride and other sulphonylureas, the following drug interactions should be considered.
- With the pharmaceutical products that are inducers and inhibitors of isoenzyme SYR2S9:
Glimepiride is metabolized via the cytochrome P450 2C9 (isoenzyme SYR2S9). In case of its simultaneous application with inductors of isoenzyme SYR2S9 (e.g. Rifampicin), hypoglycemic effects of glimepiride may decrease, while the abolition of inductors of isoenzyme SYR2S9 without dose adjustment of glimepiride may increase the risk of hypoglycemia. Simultaneous administration of inhibitors of isoenzyme SYR2S9 (e.g. Fluconazole) increases the risk of hypoglycemia and side effects of glimepiride, while the abolition of inhibitors of isoenzyme SYR2S9 without dose adjustment of glimepiride may reduce its hypoglycemic effect.
- With the pharmaceutical products reinforcing hypoglycemic effect of glimepiride:
insulin and insulin analogs, hypoglycemic agents for oral administration, angiotensin converting enzyme (ACE) inhibitors, anabolic steroids, male sex hormones, chloramphenicol, indirect anticoagulants, coumarin derivatives, cyclophosphamide, disopyramide, fenfluramine, feniramidol, fibrates, fluoxetine, guanethidine, ifosfamide, monoamine oxidase inhibitors (MAO), miconazole, fluconazole, aminosalicylic acid, pentoxifylline (high dose parenteral), phenylbutazone, azapropazone, oxyphenbutazone, probenecid, antimicrobials - quinolone derivatives, salicylates, sulfinpyrazone, clarithromycin, sulfanilamide antimicrobials, tetracyclines, tritokvalin, trofosfamide. Increased risk of hypoglycemia in case of simultaneous administration of these drugs with glimepiride and the risk of deterioration of glycemic control at their cancellation without correction of dose of glimepiride
- With the pharmaceutical products that weaken the hypoglycemic action:
acetazolamide, barbiturates, glucocorticosteroids, diazoxide, diuretics, epinephrine (adrenaline) or other sympathomimetics, glucagon, laxatives (prolonged use), nicotinic acid (high dose), estrogens, progestogens, phenothiazines, phenytoin, rifampicin, thyroid hormone drugs. The risk of weakening the hypoglycemic action of glimepiride in case of concomitant administration with these medicines and increased risk of development of hypo
- With H2-histamine receptor blockers, beta-blockers, clonidine, reserpine, guanethidine
Perhaps either increase or decrease of hypoglycemic effects of glimepiride. Careful monitoring of blood glucose levels shall be necessary.
With beta-blockers, clonidine, guanethidine and reserpine
Beta-blockers, clonidine, guanethidine and reserpine may reduce or completely eliminate the reactions of the adrenergic counter-regulation (reactions of the sympathetic nervous system as a response to hypoglycemia, aimed at increase of blood glucose concentration), which results in a weakening of manifestation of hypoglycemia (makes its development more invisible to the patient and doctor) and therefore makes its early detection and treatment difficult.
- With ethanol
Acute and chronic consumption of alcoholic beverages may, unpredictably, either reduce or enhance the hypoglycemic action of glimepiride.
- With indirect anticoagulants, coumarin derivatives
Glimepiride may both enhance and reduce the effects of indirect anticoagulants, coumarin derivatives.
- With bile acid sequestrants:
Colesevelam binds with glimepiride and reduces its absorption from the gastrointestinal tract. However, this interaction is not observed in case of administration of glimepiride at least 4 hours prior to administration of colesevelam. Therefore, glimepiride should be taken at least 4 hours prior to administration of colesevelam.
Interaction of metformin with other pharmaceutical products
Unacceptable combination
- With ethanol
The risk of lactic acidosis increases in case of acute alcohol intoxication, particularly in case of missing or insufficient food intake, presence of liver failure. Avoid drinking of alcohol (ethanol) and ethanol-containing medicines.
- With iodine-containing contrast agents
Intravascular administration of iodinated contrast agents may lead to development of renal failure, which in turn can lead to accumulation of metformin and increased risk of lactic acidosis. Metformin should be discontinued prior to the study or during the study and should not be resumed within 48 hours after it; resumption of metformin is possible only after the study, when normal parameters of renal function are obtained (see “Special Indications”).
- With antibiotics, having expressed nephrotoxic effect (gentamicin)
Increased risk of development of lactic acidosis
Combination with metformin, requiring caution
- With Corticosteroids (for systemic or local administration), beta2-stimulators and diuretics, owing hyperglycemic activity
The patient should be informed about the need for more frequent monitoring of blood glucose concentration, especially at the beginning of the combined therapy. You may need a dose adjustment of hypoglycemic medicines during administration or after discontinuation of the above-mentioned medicines.
- With antihypertensive pharmaceutical products
Antihypertensive pharmaceutical products, including ACE inhibitors, can change the blood glucose concentration. If necessary, the dose of metformin should be adjusted. Note, however, that hypoglycemia was not observed in case of administration of metformin in monotherapy in combination with ACE inhibitors.
- With phenprokoumon
Metformin may reduce the anticoagulant effect of phenprokoumon. Therefore, careful monitoring of international normalized ratio (INR) is recommended.
- With levothyroxine sodium
Levothyroxine sodium may reduce the hypoglycemic effect of metformin. We recommend monitoring of blood glucose concentration, especially at the beginning of treatment or discontinuation of treatment of thyroid hormone, if necessary, metformin dose should be adjusted.
- With the pharmaceutical products increasing
hypoglycemic action of metformin: insulin, sulfonylureas, anabolic steroids, guanethidine, salicylates (acetyl salicylic acid, etc.), betablockers (propranolol et al.) and MAO inhibitors.
In case of simultaneous administration of the above-mentioned pharmaceutical products with metformin, careful monitoring of the patient and control of blood glucose concentration may be needed, as the hypoglycemic effect of metformin may increase.
- With the pharmaceutical products that weaken the hypoglycemic action of metformin:epinephrine, glucocorticosteroids, thyroid hormones, estrogens, pyrazinamide, isoniazid, niacin, phenothiazines, thiazide diuretics, and other groups of diuretics, oral contraceptives, phenytoin, sympathomimetics, “slow” calcium channel blockers (CCBs).
In the case of simultaneous administration of the above-mentioned pharmaceutical products with metformin, careful monitoring of the patient and control of blood glucose concentration is needed, as the hypoglycemic action may weaken.
Interactions to be taken into account
- With furosemide
The clinical study on interaction of metformin and furosemide as a single dose in healthy volunteers has shown that simultaneous administration of these medicines affect their pharmacokinetic parameters. Furosemide increased Cmax of metformin in plasma by 22%, and AUC – by 15% without any significant changes in renal clearance of metformin. During administration with metformin, AUC and Cmax of furosemide were reduced by 31% and 12%, respectively, compared to the furosemide monotherapy and final half-life period was reduced by 32% without any significant changes in renal clearance of furosemide. Information is not available about interaction of metformin and furosemide in case of their long-term administration.
- With nifedipine
The clinical study on interaction of metformin and nifedipine as a single dose in healthy volunteers has shown that the simultaneous combined administration of metformin and nifedipine increases Cmax and AUC of metformin in plasma by 20% and 9%, respectively, and also increases the amount of metformin, excreted renally. Metformin has a minimum effect on the pharmacokinetics of nifedipine.
- With cationic medicines: amiloride, dikogsin, morphine, procainamide, quinidine, quinine, ranitidine, triamterene, trimethoprim and vancomycin
Cationic medicines, excreting through tubular secretion in kidney, are theoretically able to interact with metformin due to competition for general tubular transport system. Such interaction between metformin and oral cimetidine was observed in healthy volunteers in the clinical studies on interaction of metformin and cimetidine during single and repeated administration, where 60% increase in maximum plasma concentration and total blood concentration of metformin and 40% increase in total plasma and metformin AUC was shown. There were no changes in half-life during administration of the single dose. Metformin had no effect on pharmacokinetics of cimetidine. Despite the fact that such interactions remain purely theoretical (except for cimetidine), the patients should be careful monitored and correction of metformin dose and/or interacting pharmaceutical product should be carried out in case of simultaneous administration of cationic medicines, that are excreted from the body of the secretion system of the proximal tubules of kidneys.
- With propranolol, ibuprofen
In healthy volunteers, the studies of a single dose of metformin and propranolol, as well as metformin and ibuprofen have not shown the changes in their pharmacokinetic parameters.
4.6 Fertility, pregnancy and lactation
Pregnancy
Administration of the drug Glucotaj is contraindicated during pregnancy because of the possible adverse effects on intrauterine fetal development. Pregnant women and women planning pregnancy should notify the doctor about this. During pregnancy and when planning, women with impaired glucose metabolism, which cannot be corrected with diet and physical activity, must receive insulin therapy in order to maintain normal blood concentrations of blood glucose level.
Breast-feeding
In order to avoid transfer of medicine to the child’s body through breast milk, women should not take this medicine in breastfeeding period. In case of need for hypoglycemic therapy, the patient must be transferred to the insulin treatment, otherwise she must discontinue breastfeeding.
4.7 Effects on ability to drive and use machines
Speed of reactions of patients may deteriorate as a result of hyperglycemia and hypoglycemia, especially at the beginning of treatment or after a change in treatment, or in case of irregular administration of medicine. This may affect the ability required for driving of vehicles and fulfillment of other potentially hazardous activities.
The patients should be warned of the need to exercise caution when driving, especially in the case of tendency for hypoglycemia and/or reduction of severity of its precursors.
4.8 Undesirable Effects
Frequency of side effects was determined in accordance with the classification of the World Health Organization (WHO): very often (≥ 10%), often (≥ 1%,<10%); uncommon (≥0.1%,<1%); rare (≥ 0.01%,<0.1%), and very rare, including isolated reports (<0.01%), frequency not known (determination of frequency is not possible according to available data).
Glimepiride + metformin
Administration of combination of these two medicines, either as a free combination of metformin and glimepiride monotherapies, as well as a combined medicine with fixed doses of metformin and glimepiride, is characterized by the same safety profile as the administration of each of these medicines alone.
Glimepiride
Based on clinical experience with glimepiride and other data known about sulfonylureas, following adverse reactions may develop.
Impairment of metabolism and nutrition
Hypoglycemia
Hypoglycemia may develop, which may be protracted. The symptoms of development of hypoglycemia include: headache, acute sense of hunger, nausea, vomiting, weakness, fatigue, sleep disorders, restlessness, aggressiveness, poor concentration, reduced alertness and slowdown of psychomotor reactions, depression, confusion, speech disorders, aphasia, vision disorders, tremor, paresis, sensory disturbances, dizziness, helplessness, loss of self-control, delirium, convulsions, drowsiness and loss of consciousness up to coma, shallow respiration and bradycardia.
In addition, symptoms of adrenergic anti-hypoglycemic regulations may develop in response to the developing hypoglycemia, such as sweating, stickiness of skin, increased anxiety, tachycardia, increased blood pressure, sensation of heart palpitations, angina and arrhythmia. Clinical picture of severe hypoglycemic attack may resemble acute ischemic stroke. Symptoms are almost always resolved after elimination of hypoglycemia.
Visual impairment
Temporary loss of vision, particularly at the beginning of treatment due to fluctuations in blood glucose concentration. The cause of visual impairment is temporary change in swelling of the lens, depending on the of glucose concentration, due to which their refractive indications are changed.
Gastrointestinal tract impairment
Development of gastrointestinal symptoms such as nausea, vomiting, feeling of fullness, abdominal pain and diarrhea.
Liver and biliary tract impairment
In some cases, there may be hepatitis, increased activity of “hepatic” enzymes and / or cholestasis and jaundice, which may progress to fatal liver impairment, however may regress after the cancellation of glimepiride.
Blood and lymphatic system disorders Changes in the blood pattern: thrombocytopenia (rare), in some cases - leucopenia or hemolytic anemia, erythropenia, granulocytopenia, agranulocytosis or pancytopenia. After release of the medicine on the market, the cases of severe thrombocytopenia (with platelet counts less than 10.000/microliter) (the frequency is unknown) and thrombocytopenic purpura (frequency unknown) are described.
Immune system disorders
Allergic or pseudo-allergy reactions (e.g. itching, hives or rash). These reactions occur in mild form, however, may become severe with shortness of breath or a decrease in blood pressure and sometimes are progressing to shock development. In the case of hives, you should immediately inform your doctor. There is a possibility of development of cross-allergy with other sulfonylureas, sulfonamides or similar substances. Allergic vasculitis may develop in some cases.
Skin and subcutaneous tissue disorders
Photosensitivity may develop in some cases.
Laboratory and instrumental dataHyponatremia may develop in some cases.
Metformin
Metabolism and nutrition disorders
Lactic acidosis (very rare: 0.03 cases per 1000 patient a year) (see - “Special indications”).
Gastrointestinal tract disorders
Gastrointestinal symptoms (nausea, vomiting, diarrhea, abdominal pain, flatulence, bloating and loss of appetite) - the most common reaction in case of metformin monotherapy (very often: more than 10%), these symptoms are particularly common at the beginning of treatment and resolve spontaneously while continuing treatment. In some cases, temporary reduction in dose may be useful. In order to prevent development of such reactions, it is recommended to divide the daily dose (if it exceeds 1 mg glimepiride and 250 mg metformin) into 2 doses. Due to the fact that the development of gastrointestinal symptoms is depended on dose at the beginning of treatment, gradual increase in dose during its selection or its reception after a meal can also reduce these symptoms.
Since severe diarrhea and (or) vomiting can lead to dehydration and prerenal azotemia, it is recommended to stop taking of Glucotaj when they appear. Appearance of non-specific gastrointestinal symptoms in patients with diabetes mellitus type 2, with a stabilized condition on the background of administration of Amaryl ®M, can be connected not only with the therapy, but also with intercurrent illness or lactic acidosis development. At the beginning of the treatment with metformin (often: approximately 3% of patients) may cause an unpleasant or “metallic” taste in the mouth, which usually disappears spontaneously.
Skin and subcutaneous tissue disorders
Very rare (<0.01%) - erythema in patients with hypersensitivity, pruritus, rash.
Blood and lymphatic system disorders
Anemia, hemolytic anemia (frequency is unknown), leucocytopenia or thrombocytopenia. If a patient has megaloblastic anemia, the possibility of reduction of absorption of vitamin B12, associated with administration of metformin, should be considered (see below).
Liver and biliary tract disorders
Deviation from the norm of the functional “liver” tests or hepatitis, which are subjected to reverse development with discontinuation of metformin.
Laboratory and instrumental data
Reduction of concentration of thyroid-stimulating hormone in patients with hypothyroidism (frequency is unknown) (see “Special indications”).
Hypomagnesemia (diarrhea) (frequency is unknown). Reduction of concentration of vitamin B12 in blood: in <0.01% of patients treated with metformin for a long time, there was a decrease in absorption of vitamin B12, usually accompanied by a clinically insignificant decrease in its serum concentration.
Nervous system disorders
Encephalopathy (frequency is unknown).
In post-marketing administration of metformin by the patients with vitamin B12 deficiency, cases of peripheral neuropathy were observed (frequency is unknown) (see “Special indications”).
Skin and subcutaneous tissue disorders Photosensitivity (frequency is unknown).
In case of development of the above or other side effects, the patient should immediately notify the doctor.
As some adverse reactions, including hypoglycemia, lactic acidosis, hematological disorders, severe allergic and pseudoallergy reactions and liver failure may threaten the patient’s life, in case of development of such reactions; the patient should immediately inform his/her doctor and stop the administration of medicine until acceptance of appropriate instructions from the doctor.
4.9 Overdose
Since Glucotaj contains glimepiride, overdose (such as acute and chronic administration of the medicine in high doses) can cause severe, life-threatening hypoglycemia.
As soon as glimepiride overdose is determined, you should immediately inform your doctor. Until medical assistance arrives, the patient should immediately take sugar, if possible, in the form of dextrose (glucose).
It is necessary to conduct gastric lavage and give activated charcoal to the patients, who have taken a life-threatening amount of glimepiride.
Sometimes, hospitalization is required as a preventive measure.
Light hypoglycemia without loss of consciousness or neurological manifestations should be treated by oral administration of dextrose (glucose), correction dose of Amaril®M and\or the patient’s diet.
Significant overdose and serious hypoglycemic reactions with the symptoms such as loss of consciousness or other serious neurological disorders are critical conditions, requiring immediate hospitalization. In case of unconscious state, the patient should be given concentrated solution of glucose (dextrose) intravenously, for example, for adults the dose starts with 40 ml of 20% glucose (dextrose).
Glucagon administration, for example, at a dose of 0.5 to 1 mg intravenously, subcutaneously or intramuscularly, is considered as an alternative treatment for adult patients.
After rapid administration of glucose, it is necessary to conduct glucose infusion at a low concentration as long as the doctor is sure that the threat of resumption of hypoglycemia has passed.
Blood glucose concentrations should be carefully monitored for at least 24-48 hours, as hypoglycemia may recur after apparent clinical recovery.
Risk of recurrence of hypoglycemia in severe cases with a prolonged course may persist for several days.
In case of treatment of hypoglycemia in children with accidental administration of glimepiride, the dose of administered dextrose should be very carefully adjusted under the constant control of blood glucose concentration, due to potential development of dangerous hyperglycemia.
Metformin overdose
Hypoglycemia was not observed in case of administration of 85 g metformin, although in some cases there was lactic acidosis.
Significant metformin overdose or accompanying risks to the patient may lead to development of lactic acidosis, requiring urgent medical treatment in a hospital.
The most efficient way to remove lactate and metformin from the body of the patient is hemodialysis. With good hemodynamics, metformin may be eliminated via hemodialysis with a clearance of up to 170 ml/min.
Acute pancreatitis may develop in case of metformin overdose.
5 Pharmacological properties
5.1 Pharmacodynamic properties
Glucotaj is a combined hypoglycemic medicine, which is composed of glimepiride and metformin.
Pharmacodynamics of glimepirideGlimepiride, one of the active substances of Glucotaj, is an oral hypoglycemic medicine - sulfonylureas of the III generation.
Glimepiride stimulates secretion and release of insulin from the pancreas beta-cells (pancreatic effect), improves sensitivity of peripheral tissues (muscle and fat) to the action of endogenous insulin (extrapancreatic action).
Effect on insulin secretion
Sulfonylureas increase insulin secretion by closing the ATP-dependent potassium channels, located in the cytoplasmic membrane of pancreatic beta-cells. By closing the potassium channels, they cause depolarization of the beta-cells, thus facilitating opening of calcium channels and increasing of transmission of calcium into the cells. Glimepiride is bounded and unbounded from the protein of pancreatic beta cells at a high replacement rate of (mol. mass - 65 kD/SURX), which is associated with the ATP-dependent potassium channels, however it is different from the binding sites of conventional sulfonylureas (protein with mol. mass - 140 kD/SUR1).
This process leads to release of insulin by exocytosis, and the amount of secreted insulin is significantly lesser than with sulfonylureas of II generation (e.g. glibenclamide).
Minimum stimulating effect of glimepiride on insulin secretion is provided and there is a lower risk of development of hypoglycemia.
Extrapancreatic activity
As with traditional sulfonylureas, but to a greater extent, glimepiride has pronounced extrapancreatic effects (reduction of insulin resistance, antiatherogenic, antiplatelet and antioxidant action).
Utilization of glucose by peripheral tissues (fat and muscle) occurs via specific transporter proteins (GLUT1 and GLUT4), located in the cell membranes.
Transportation of glucose in these tissues in diabetes mellitus type 2 is limited in rate of glucose utilization stage. Glimepiride very rapidly increases the number and activity of molecules, glucose transporter (GLUT1 and GLUT4), which leads to an increase in glucose uptake by peripheral tissues.
Glimepiride has a weak inhibitory effect on ATP-sensitive potassium channels of cardiomyocytes. Upon administration of glimepiride, the ability of metabolic adaptation to myocardial ischemia is preserved.
Glimepiride increases the activity of phospholipase C, which results reduction of intracellular calcium concentration in muscle and fat cells, causing decrease in the activity of proteinkinaseA, which in turn, leads to lead to stimulation of glucose metabolism.
Glimepiride inhibits hepatic glucose output by increasing the intracellular concentration of fructose-2,6-bisphosphate, which in turn inhibits gluconeogenesis.
Glimepiride selectively inhibits cyclooxygenase and reduces conversion of arachidonic acid to thromboxane A2, important endogenous factor for platelet aggregation.
Glimepiride reduces the lipid content, significantly decreases lipid peroxidation and promotes its anti-atherogenic effect.
Glimepiride increases the content of endogenous α-tocopherol, activity of catalase, glutathione peroxidase and superoxide dismutase, thereby reducing the severity of oxidative stress, always presented in the body of the patient with diabetes mellitus type 2.
Pharmacodynamics of metformin
Metformin is a hypoglycemic medicine from the biguanide group. Its hypoglycemic effect is possible only under condition of preservation of insulin secretion (although reduced). Metformin has no effect on the beta-cells of the pancreas and does not increase secretion of insulin. Metformin at therapeutic doses do not cause hypoglycemia in humans. The mechanism of action of metformin is not yet completely learnt. It is assumed that metformin may potentiate the effects of insulin or that it can increase the effects of insulin receptors in peripheral areas. Metformin increases insulin sensitivity due to increase in the number of insulin receptors on cell surface membranes. Besides metformin inhibits gluconeogenesis in the liver, reduces formation of free fatty acids and fat oxidation, reduces the concentration of triglyceride (TG) and low-density lipoproteids (LDL) and very low-density lipoprotein (VLDL) in blood. Metformin slightly reduces appetite and decreases absorption of carbohydrates in the intestine. It improves blood fibrinolytic properties due to suppression of tissue plasminogen activator inhibitor.
5.2 Pharmacokinetic properties
Pharmacokinetics of glimepiride
With multiple daily dose of 4 mg glimepiride, maximum serum concentration (Cmax) is achieved after about 2.5 hours and is 309 ng / ml; there is a linear relationship between dose and Cmax, as well as between the dose and AUC (area under plasma “concentration – time” curve).
When administered, bioavailability of glimepiride is almost complete. Food intake has no significant effect on absorption, with the exception of a slight slow-down of the rate of absorption. Glimepiride is characterized by a very low distribution volume (approximately 8.8 liters), approximately equal to the albumin distribution volume, high plasma protein binding level (99%) and low clearance (about 48 ml/min).
After a single oral administration of glimepiride, 58% of the dose is excreted by the kidneys (as metabolites) and 35% of the dose is excreted through the intestines. Half-life in case of plasma concentrations of glimepiride in plasma, corresponding to the multiple administration, is 5-8 hours. After administration of high dose, half-life increases slightly.
In urine and faeces two inactive metabolites are revealed, resulting the metabolism in the liver, one of them is hydroxy derivative, and the other - carboxy derivative. After oral administration of glimepiride, terminal half-life of these metabolites is 3-5 hours and 5-6 hours, respectively. Glimepiride is excreted in breast milk and crosses the placental barrier. Glimepiride poorly crosses the blood-brain barrier.
Comparison of single and multiple (2 times daily) administration of glimepiride did not reveal significant differences in the pharmacokinetic parameters and their variability between patients was insignificant. Significant accumulation of glimepiride was absent.
Pharmacokinetic parameters of glimepiride are the same for patients of different genders and various ages. In patients with impaired renal function (low creatinine clearance) tended to increase clearance of glimepiride and decrease in its average concentrations in the blood serum, which is likely caused by a more rapid clearance of glimepiride due to its lower binding to plasma proteins. Thus there is no additional risk of accumulation of glimepiride in such categories of patients.
Pharmacokinetics of metformin
Metformin is absorbed from the gastrointestinal tract adequately after oral administration. Absolute bioavailability is 50-60%. Cmax, composed of average 2 mg/ml, is reached after 2.5 hours. In case of simultaneous food intake, absorption of metformin is reduced and slowed down.
Metformin is rapidly distributed into the tissue, practically does not bind to plasma proteins. It is metabolized to a very small extent and excreted by the kidneys. The clearance in healthy subjects is 440 ml/min (4 times greater than that of creatinine), indicating presence of active tubular secretion of metformin. Half-life of metformin is approximately 6.5 hours. There is a risk of metformin accumulation in case of renal insufficiency.
Pharmacokinetics Glucotaj with the fixed dose of glimepiride and metformin
In case of administration of fixed dose of the combined drug Glucotaj (tablet containing glimepiride 2 mg + metformin 500 mg), Cmax and AUC values correspond to bioequivalence criteria when compared to the same parameters in case of administration of the same combination as separate preparations (tablet of glimepiride 2 mg and metformin 500 mg).
In addition, dose-proportional increase of Cmax and AUC of glimepiride was shown by increasing the dose from 1 mg to 2 mg in the combined fixed-dose preparations with a constant dose of metformin (500 mg) in the composition of these preparations.
No other significant differences are observed in safety, including profile of adverse effects in patients taking the drug Glucotaj 1 mg +500 mg, and the patients taking the drug Amaril®M 2 mg +500 mg.
6 Pharmaceutical particulars
6.1 List of excipients
Excipients: Lactose monohydrate - 50 mg, Carboxymethyl starch sodium - 15 mg, Povidone K30 - 25 mg Microcrystalline cellulose - 50 mg, Crospovidone - 10 mg, Magnesium stearate - 5 mg; Film coating: Hypromellose - 9.4 mg, Macrogol-6000 - 1.7 mg, Titanium dioxide (E 171) - 1.7 mg, Carnauba wax - 0.2 mg.
6.2 Incompatibilities
Store at temperatures not above 30 ° C.
Keep out of the reach of children.
6.3 Shelf life
3 years. Do not use the medicine after the expiry date stated on the package.
6.4 Special precautions for storage
Tablets, film-coated 2 mg + 500 mg 10 tablets in PVC / aluminum blister. 3 blisters with instruction on use in a cardboard box
7 Manufacturer:
Manufactured in India by:
TAJ PHARMACEUTICALS LTD,
220, Mahagujarat Ind. Estate, Moraiya,
Tal. Sanand , Dist. Ahmedabad,
Gujarat, INDIA.
Click here for Download pdf of patient informationClick here for Download pdf of prescribing information
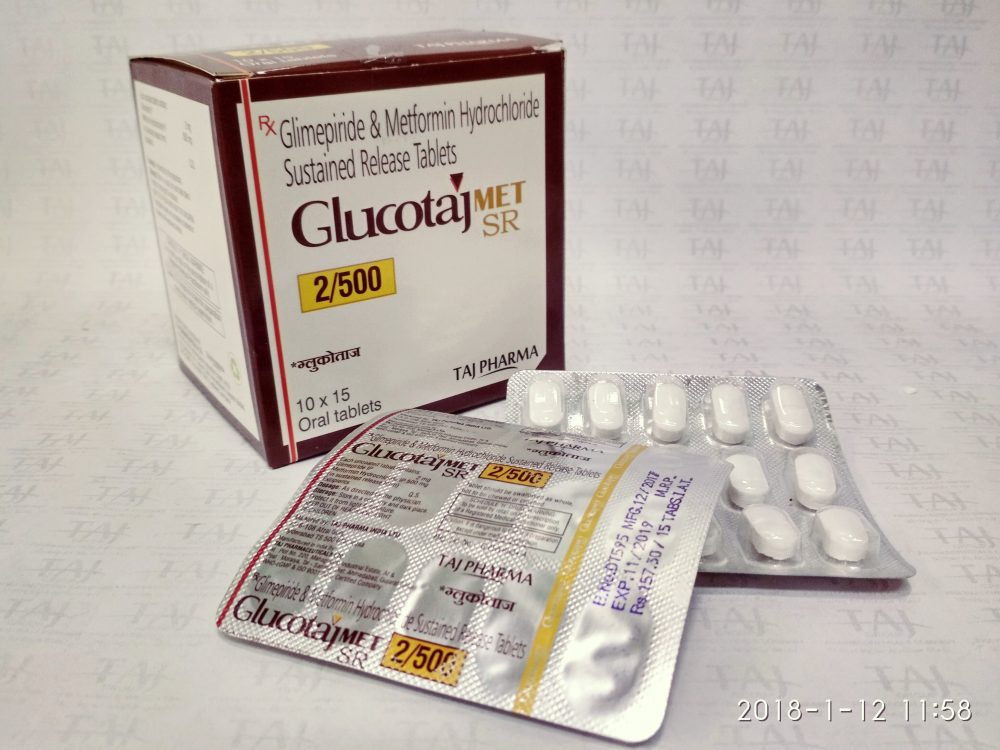
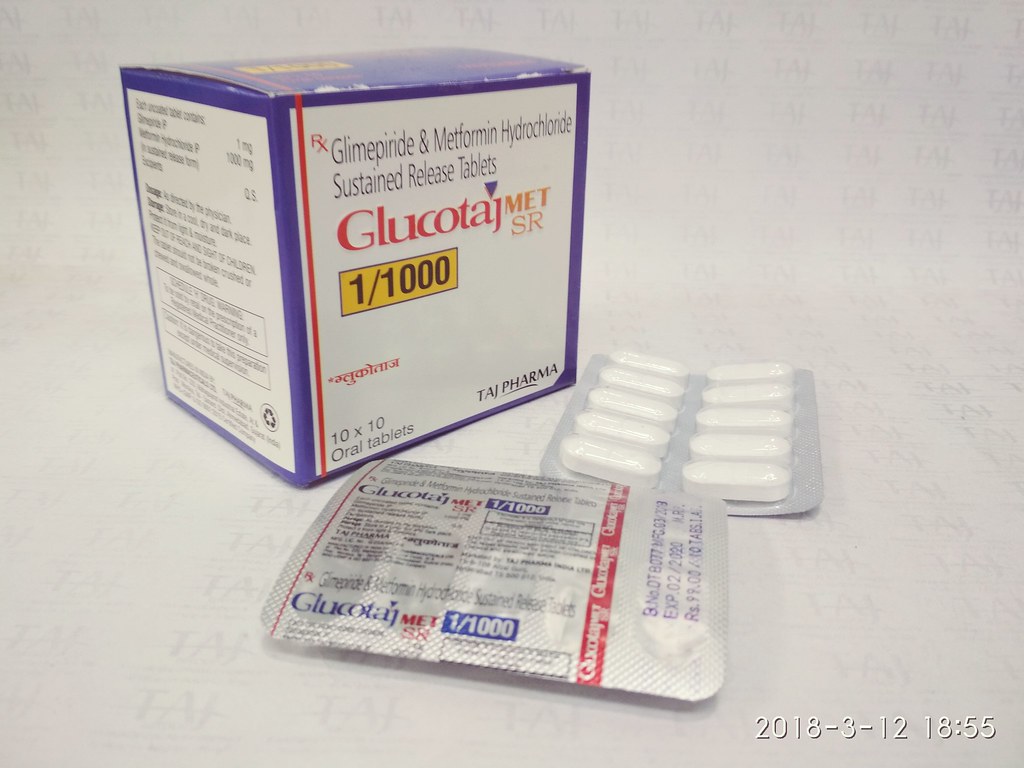
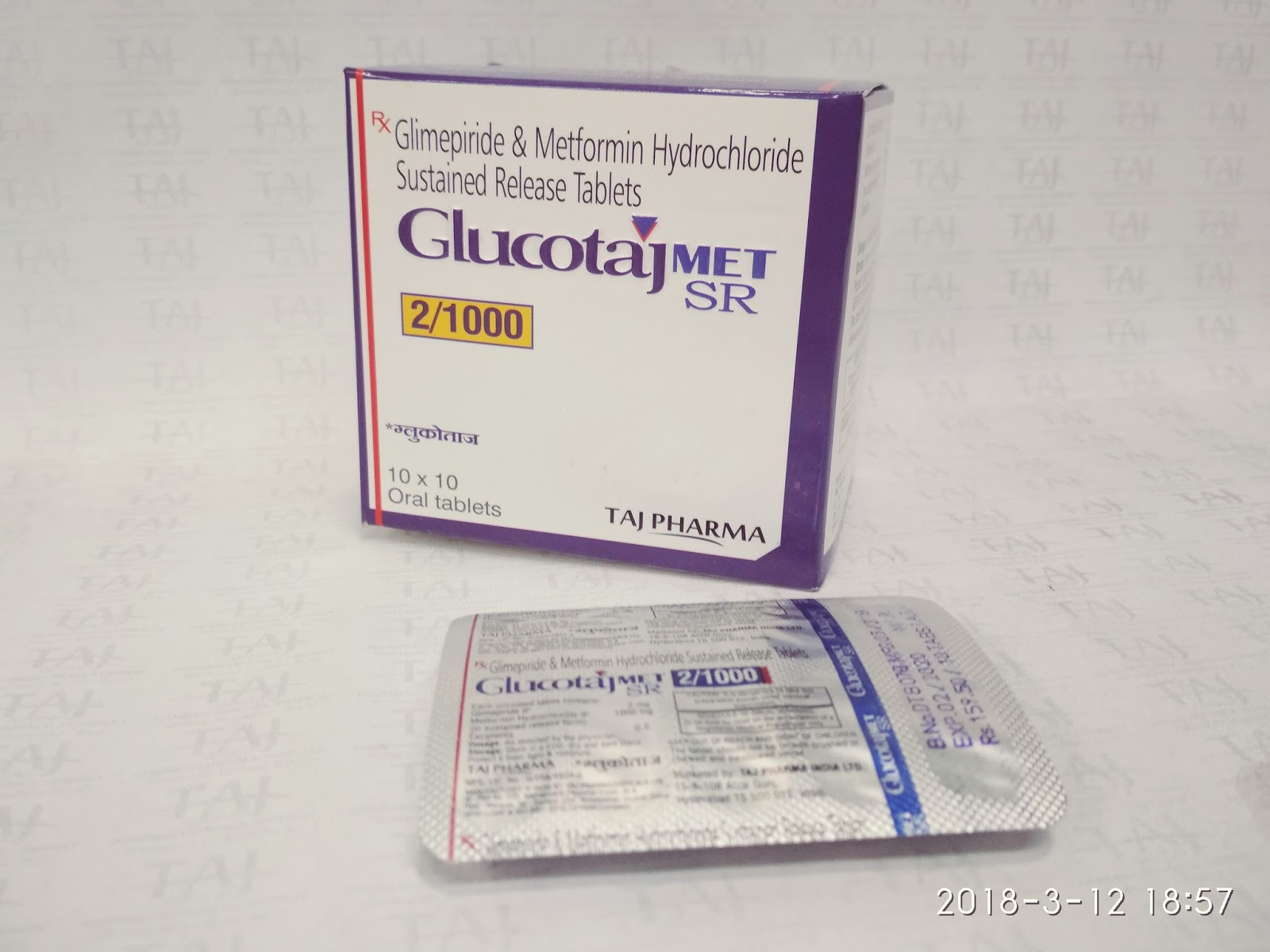
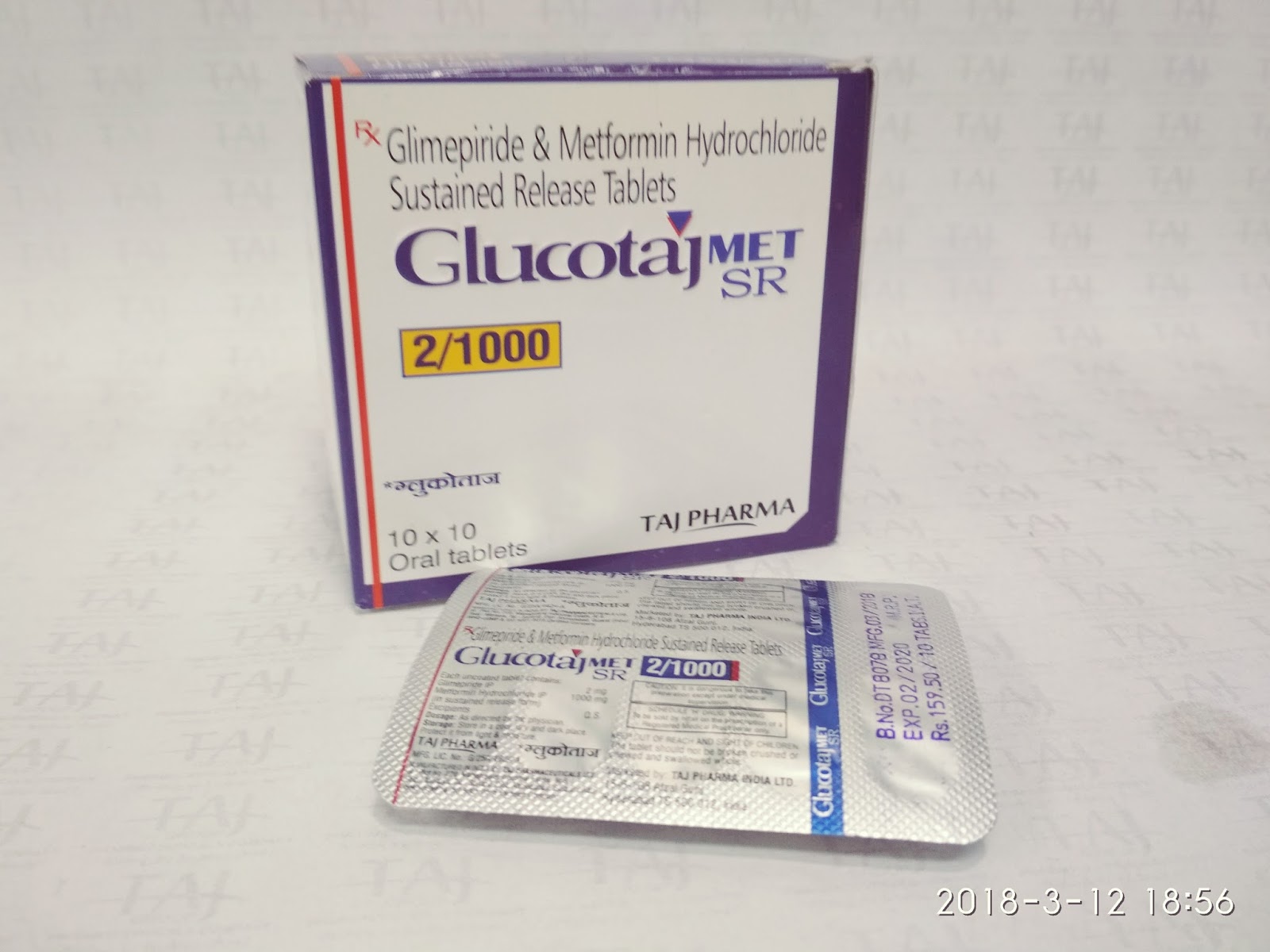
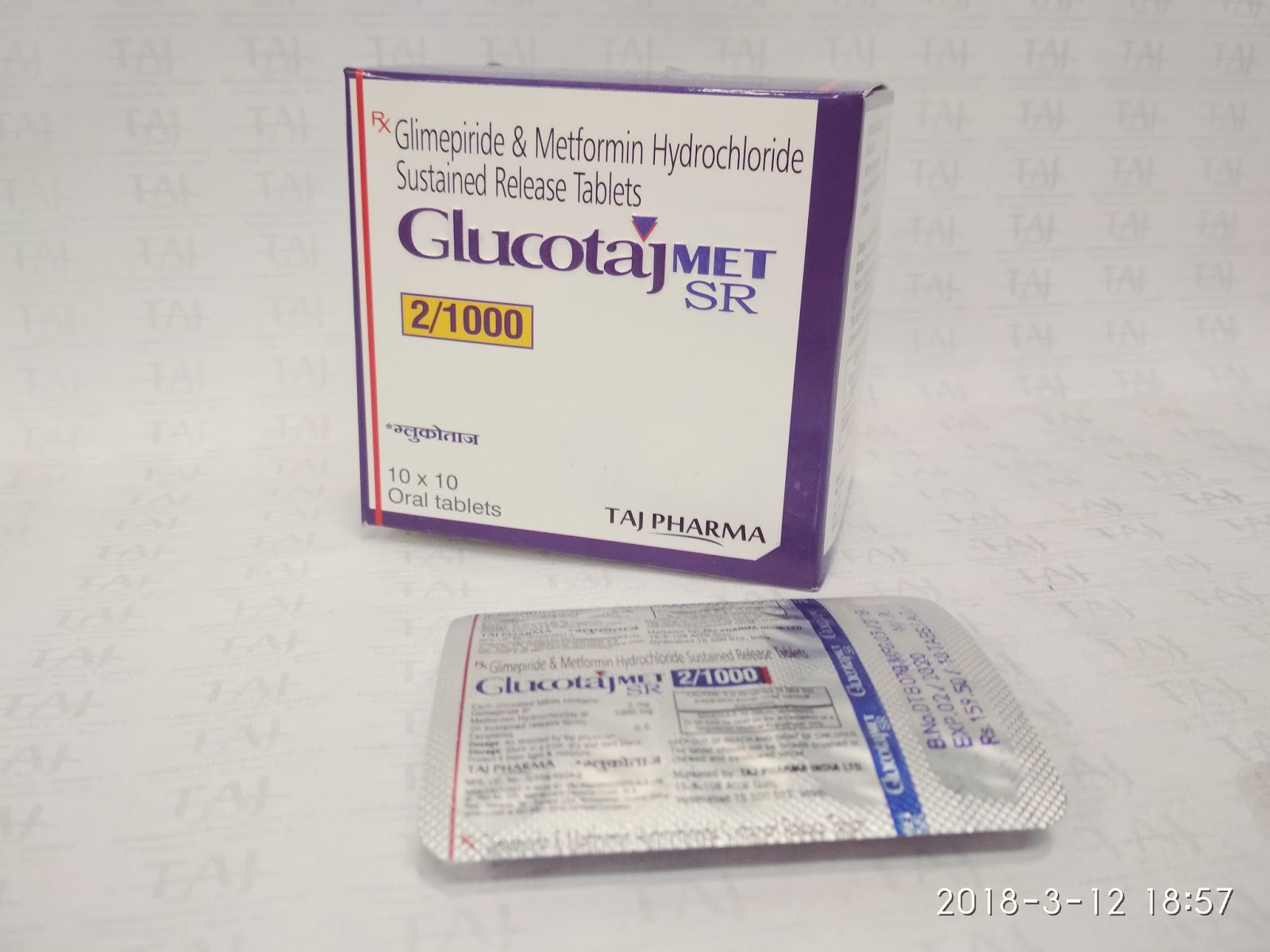
Glucotaj Image Gallery
Here you can see the images of Metformin Hydrochloride Prolonged Release and Glimpiride Tablets.
Our Partners
A dream for new world Anchored in India and committed to its traditional values of leadership with trust, the Taj Pharma Group is spreading its footprint globally through excellence and innovation. Taj Pahrma







Life is the underlying purpose of everything we do at Taj Pharma Group. We are committed to developing a distinguished generics pharmaceuticals business.
Taj Pharma is one of the leading generic pharmaceutical company in India. We hold top positions in different established markets and gradually building a strong presence in many emerging generics markets. We have eight manufacturing sites under flagship in India to support our market standing.
Copyright © Taj Pharmaceuticals Limited. All rights reserved. by Taj Pharma Group India.
Note: This site contains medical information that is intended for doctors or medical practitioner only and is not meant to substitute for the advice provided by a medical professional. Always consult a physician if you have health concerns. Use and access of this site is subject to the terms and conditions as set out in our Privacy Policy and Terms of Use. Copyright © Taj Pharmaceuticals Limited (India), All Rights Reserved.